Cortisone Rash After Injection: Causes, Symptoms, And Treatment Options
A cortisone rash after injection can be an unexpected and concerning side effect for many patients undergoing corticosteroid treatments. While cortisone injections are commonly used to reduce inflammation and pain in various medical conditions, some individuals may experience adverse reactions, including skin rashes. These rashes can range from mild irritation to more severe allergic reactions, making it essential for patients and healthcare providers to understand the underlying causes and appropriate management strategies. This article delves into the complexities of cortisone rashes, exploring their potential triggers, symptoms, and effective treatment options. By providing comprehensive information backed by medical expertise and reliable sources, we aim to empower readers with the knowledge needed to navigate this condition confidently.
Corticosteroids, such as cortisone, play a crucial role in managing inflammatory conditions like arthritis, tendonitis, and certain skin disorders. These powerful medications work by mimicking the effects of hormones naturally produced by the adrenal glands, effectively reducing inflammation and suppressing the immune system's response. However, like any medical treatment, cortisone injections carry potential risks and side effects. Among these, the development of a rash at the injection site has emerged as a notable concern for both patients and medical professionals. Understanding the mechanisms behind this reaction is vital for proper diagnosis and treatment.
As we explore the topic of cortisone rash after injection, we will examine the various factors that contribute to this condition, including individual patient characteristics, injection techniques, and medication formulations. The article will provide detailed information on how to identify and differentiate between normal post-injection reactions and more serious complications. Furthermore, we will discuss evidence-based treatment approaches and preventive measures, drawing from current medical guidelines and expert recommendations. Whether you're a healthcare professional seeking to enhance your knowledge or a patient looking for reliable information, this comprehensive guide aims to address all aspects of cortisone-related skin reactions.
Read also:Understanding The Zodiac Year 1965 Insights And Meanings
Table of Contents
- Understanding Cortisone Injections
- Common Side Effects of Cortisone Injections
- Causes of Cortisone Rash After Injection
- Symptoms and Diagnosis of Cortisone Rash
- Treatment Options for Cortisone Rash
- Prevention Strategies
- When to See a Doctor
- Long-Term Management and Considerations
- Patient Stories and Experiences
- Conclusion and Final Thoughts
Understanding Cortisone Injections
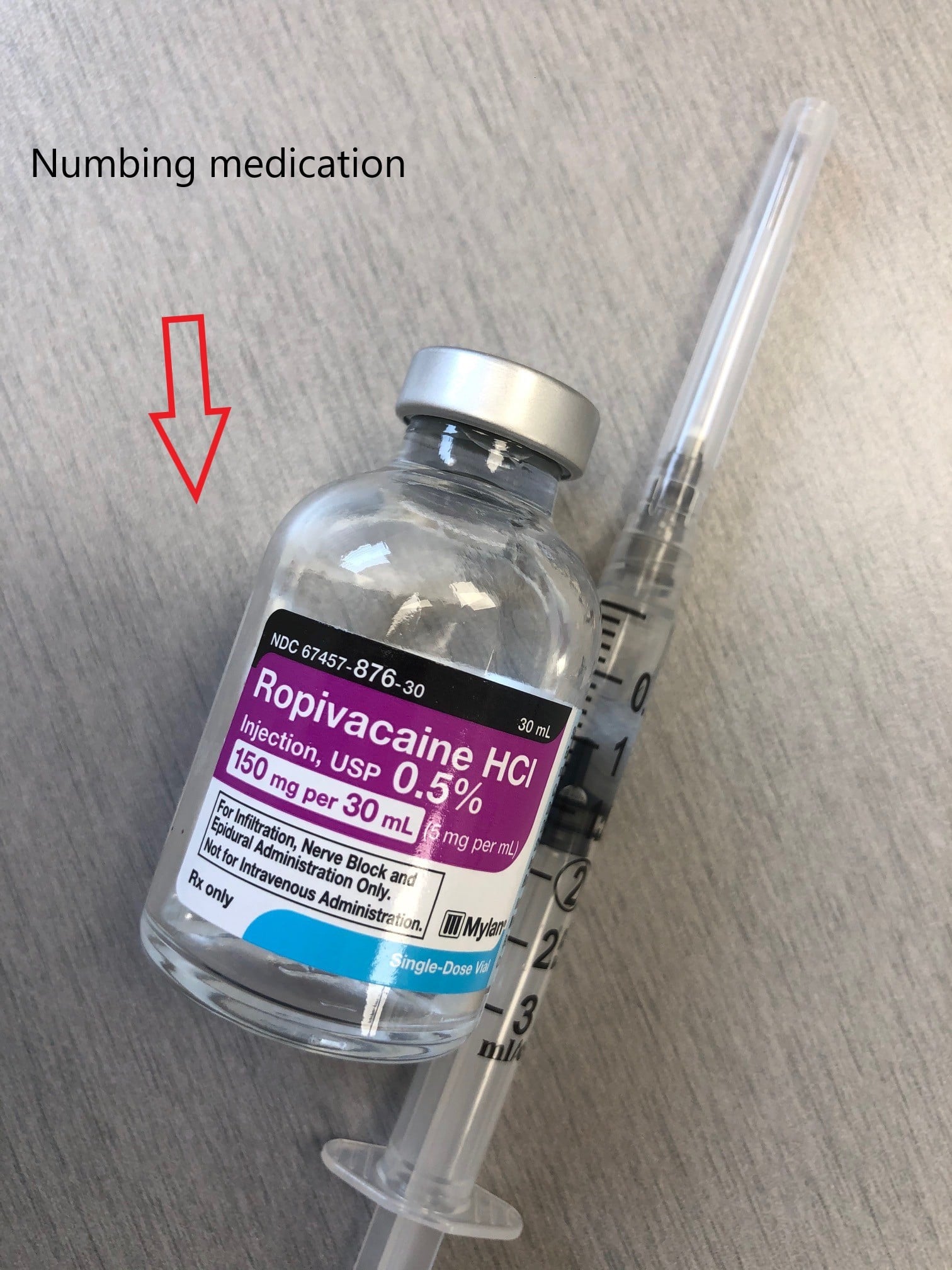
Cortisone injections, also known as corticosteroid injections, represent a cornerstone in modern medical treatment for various inflammatory conditions. These injections typically contain synthetic versions of cortisol, a hormone naturally produced by the adrenal glands. The primary function of cortisone is to reduce inflammation and suppress the immune system's response, making it particularly effective in managing conditions such as rheumatoid arthritis, osteoarthritis, tendinitis, bursitis, and certain skin disorders. When administered directly into affected joints or tissues, cortisone can provide targeted relief, often resulting in significant pain reduction and improved mobility.
The administration of cortisone injections requires precise medical expertise and careful consideration of several factors. Healthcare providers must evaluate the patient's medical history, current medications, and specific condition before determining the appropriate dosage and injection site. Common injection sites include joints (such as knees, shoulders, and hips), soft tissues (like tendons and bursae), and specific trigger points in muscles. The procedure itself is relatively quick, typically lasting only a few minutes, and is often performed in outpatient settings. While the immediate effects of cortisone can be dramatic, with some patients experiencing rapid pain relief, the duration of these effects can vary from weeks to months, depending on individual response and the specific condition being treated.
Despite their effectiveness, cortisone injections are not without limitations and potential risks. The frequency of injections is carefully controlled, with most medical guidelines recommending no more than three to four injections per year in a single joint. This restriction is due to potential long-term effects on joint tissues and cartilage. Additionally, while cortisone can provide temporary relief, it does not address the underlying cause of inflammation. Therefore, it is often used in conjunction with other treatments, such as physical therapy or disease-modifying medications, to achieve optimal outcomes. Understanding these fundamental aspects of cortisone injections is crucial for both patients and healthcare providers in making informed decisions about their use and managing expectations regarding results and potential side effects.
Common Side Effects of Cortisone Injections
While cortisone injections are generally considered safe and effective when administered properly, they can produce several common side effects that patients should be aware of. The most frequently reported immediate reaction is localized pain or discomfort at the injection site, which typically resolves within a few days. This discomfort may be accompanied by slight swelling or bruising, which are normal responses to the injection process itself. Some patients may also experience a temporary increase in pain, known as a "steroid flare," which usually subsides within 24 to 48 hours and can be managed with ice application and over-the-counter pain relievers.
Other common side effects include skin discoloration at the injection site, which may appear as either lightening or darkening of the skin, and temporary elevation of blood sugar levels, particularly concerning for patients with diabetes. In some cases, patients may notice a reduction in skin thickness or changes in fat distribution around the injection area, especially with repeated treatments. These effects are typically more pronounced with frequent or improperly administered injections. Less commonly, patients may experience facial flushing, a temporary reaction that occurs shortly after the injection and usually resolves within a few hours. While these side effects are generally mild and manageable, they highlight the importance of proper injection technique and careful consideration of patient-specific factors before proceeding with treatment.
Causes of Cortisone Rash After Injection
The development of a rash following a cortisone injection can stem from several distinct mechanisms, each requiring specific attention and management. While relatively uncommon, these reactions can occur in patients receiving corticosteroid injections and may indicate underlying sensitivities or complications that need to be addressed. Understanding the primary causes of cortisone rash is crucial for both prevention and appropriate treatment.
Read also:Razor Haircuts For Medium Length Hair The Ultimate Guide To Stylish And Modern Looks
Allergic Reactions
Allergic reactions to cortisone injections represent one of the most significant causes of post-injection rashes. Although rare, some individuals may develop hypersensitivity to the corticosteroid compound itself or to other components present in the injection formulation, such as preservatives or stabilizers. These allergic reactions can manifest as localized or widespread skin eruptions, often accompanied by itching, redness, and swelling. In severe cases, patients may experience systemic symptoms including difficulty breathing, facial swelling, or anaphylaxis, requiring immediate medical attention. The risk of allergic reactions increases in patients with known drug sensitivities or those who have previously experienced adverse reactions to corticosteroid treatments.
Local Irritation
Local irritation at the injection site represents another common cause of cortisone rash development. This reaction typically occurs due to several factors, including improper injection technique, rapid administration of the medication, or the physical properties of the corticosteroid preparation. Some cortisone formulations may have a higher pH or contain crystalline particles that can irritate local tissues, leading to inflammatory responses and subsequent rash formation. Additionally, the volume and pressure of the injection can cause mechanical damage to surrounding tissues, triggering an inflammatory cascade that results in skin reactions. Unlike allergic reactions, these irritation-induced rashes usually remain localized and tend to resolve more quickly with appropriate care and management.
Symptoms and Diagnosis of Cortisone Rash
Identifying a cortisone rash requires careful observation of specific symptoms and distinguishing characteristics that differentiate it from other post-injection reactions or skin conditions. The appearance of a cortisone rash typically develops within hours to days following the injection and presents as a distinct pattern of skin changes. Common visual characteristics include raised, red patches or welts at the injection site, sometimes accompanied by a spreading pattern that may extend several centimeters beyond the immediate injection area. The rash may appear as a combination of hives, eczema-like patches, or more generalized redness and swelling, depending on the underlying cause.
Accompanying symptoms often include intense itching, burning sensations, or localized warmth at the affected area. In some cases, patients may experience tenderness or pain that differs from the normal post-injection discomfort. The severity of symptoms can vary significantly, ranging from mild irritation to more pronounced reactions that may affect daily activities. It's crucial to note the timing of symptom onset, as immediate reactions suggest different underlying causes compared to delayed responses. Healthcare professionals typically employ a combination of clinical evaluation, patient history, and sometimes patch testing to accurately diagnose cortisone rash and rule out other potential causes such as infection or allergic contact dermatitis.
Treatment Options for Cortisone Rash
Managing a cortisone rash requires a systematic approach that addresses both immediate symptoms and underlying causes. The treatment strategy typically begins with conservative measures and progresses to more intensive interventions based on the severity of the reaction and patient response. Effective treatment plans often combine multiple approaches to ensure comprehensive management of the condition.
Topical Treatments
Topical treatments form the foundation of cortisone rash management, offering targeted relief directly at the affected site. Mild cases often respond well to over-the-counter hydrocortisone creams, which help reduce inflammation and alleviate itching. For more persistent or severe reactions, prescription-strength topical corticosteroids may be necessary, though their use must be carefully monitored to prevent further irritation. Antihistamine creams can provide additional relief from itching and help control allergic reactions. In cases where significant skin irritation is present, healthcare providers may recommend emollients or barrier creams to protect the skin and promote healing. It's crucial to follow specific application instructions and avoid excessive use of topical treatments, as overuse can sometimes exacerbate the condition.
Oral Medications
When topical treatments prove insufficient, oral medications may be prescribed to manage more severe cortisone rash reactions. Antihistamines, particularly second-generation options like loratadine or cetirizine, are commonly used to control allergic symptoms and reduce itching. In cases where significant inflammation persists, short courses of oral corticosteroids may be prescribed, though this approach requires careful consideration due to potential interactions with the original injection treatment. For patients experiencing severe allergic reactions, healthcare providers may recommend leukotriene receptor antagonists or other systemic medications to address underlying immune responses. Pain management may also be necessary, with acetaminophen or non-steroidal anti-inflammatory drugs (NSAIDs) prescribed as needed to control discomfort while the rash resolves.
Prevention Strategies
Preventing cortisone rash requires a proactive approach that combines careful preparation, precise administration techniques, and thorough patient education. One of the most effective preventive measures involves conducting comprehensive patient assessments before injection, including detailed allergy history reviews and skin sensitivity evaluations. Healthcare providers should carefully document any previous adverse reactions to medications or injections and consider performing patch tests when there's suspicion of potential sensitivity. Proper injection technique plays a crucial role in prevention, with emphasis on using the correct needle size, appropriate injection speed, and optimal medication formulation for each patient's specific condition.
Patient education serves as another vital component of prevention strategies. Patients should be thoroughly informed about potential side effects and instructed to report any unusual reactions immediately. Pre-treatment protocols may include applying topical anesthetics or using ice packs to minimize local irritation. Additionally, healthcare providers should carefully consider the timing and frequency of injections, allowing adequate recovery periods between treatments to reduce cumulative irritation risks. For patients with known sensitivities, alternative treatment options or modified corticosteroid formulations may be explored to minimize the risk of rash development.
When to See a Doctor
Recognizing when to seek medical attention for a cortisone rash is crucial for ensuring proper management and preventing potential complications. While mild reactions can often be managed with home care, certain warning signs indicate the need for immediate medical evaluation. Patients should seek prompt medical attention if they experience difficulty breathing, facial swelling, or throat tightness, as these symptoms may indicate a severe allergic reaction requiring emergency treatment. Widespread rash development, particularly when accompanied by fever or systemic symptoms, also warrants urgent medical assessment to rule out serious complications or underlying conditions.
Other concerning signs that necessitate professional evaluation include rash
Ratatouille Brothers: The Unlikely Heroes Of Culinary Creativity
Traits Of Gemini Man: Unveiling The Multifaceted Personality
1995 Chinese Zodiac: Unveiling The Year Of The Wood Pig
Cortisone Injection Complete Orthopedics Multiple NY Locations

Cortisone shot in foot, does it help? District Foot & Ankle